Calciphylaxis
*This is a working document. Last updated: 5/7/2020
What is Calciphylaxis?
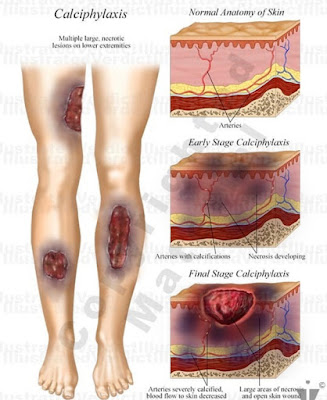
 Calciphylaxis (kal-sih-fuh-LAK-sis) is a serious, uncommon disease in which calcium accumulates in small blood vessels of the fat and skin tissues (Source: Mayo Clinic). Calciphylaxis is also called calcific uraemic arteriolopathy or calcific vasculopathy (Source: DermNetNZ). Calciphylaxis is a poorly understood and highly morbid syndrome of vascular calcification and skin necrosis (Source: MedScape). There is an 80% mortality rate.
Calciphylaxis (kal-sih-fuh-LAK-sis) is a serious, uncommon disease in which calcium accumulates in small blood vessels of the fat and skin tissues (Source: Mayo Clinic). Calciphylaxis is also called calcific uraemic arteriolopathy or calcific vasculopathy (Source: DermNetNZ). Calciphylaxis is a poorly understood and highly morbid syndrome of vascular calcification and skin necrosis (Source: MedScape). There is an 80% mortality rate.Calciphylaxis causes blood clots, painful skin ulcers and may cause serious infections that can lead to death. People who have Calciphylaxis usually have kidney failure and are on dialysis or have had a kidney transplant. The condition can also occur in people without kidney disease (Source: Mayo Clinic).
Epidemiology: (study of diseases in populations of humans or other animals, specifically how, when and where they occur)
Calciphylaxis is an uncommon condition that affects 1-4% of the population with ESRD.
Although the disease may affect persons of any race, it appears to be more prevalent in whites. Females are affected more often than males, with a female-to-male ratio of approximately 3:1. Females also appear to be more commonly affected with nonuremic calciphylaxis.
Calciphylaxis has been reported in individuals ranging in age from 6 months to 83 years. From a large series of patients, a mean patient age of 48 years (±16 y) has been calculated. Individuals seemingly more predisposed are younger patients who have had a longer duration of renal replacement therapy.
(Source: MedScape)
What are the signs and symptoms of Calciphylaxis?
- A lot of Pain
- Large purple net-like patterns on skin
- Deep, very painful lumps that ulcerate creating open sores with black-brown crust that fails to heal — typically in skin areas with high fat content, such as the stomach and thigh, although they can occur anywhere
- Infections from wounds that don't heal
(Source: Mayo Clinic)
Be careful and wary of initial diagnosis: Calciphylaxis appears very much like flesh eating because the calcium is clogging your blood vessels under your skin preventing blood flow to the skin, so the skin dies off. It literally starts to form a wound, turns black, and the skin just dies because there is no healthy blood flow to it. Gangrene/Flesh Eating Disease could present similarly. Speak up and advocate for yourself if you disagree with your medical team or have any concerns. They are human and humans are fallible.
Stages of Calciphylaxis:
The development of Calciphylaxis goes through two phases: (1) a silent phase where vascular calcifications are formed in the media with intimal hyperplasia of dermal and hypodermic arterioles, and then (2) a phase of microcirculatory decompensation (the failure of an organ to compensate for the functional overload blood flow through the smallest vessels in the circulatory system, i.e. arterioles, venules, shunts and capillaries) which corresponds to thrombosis ischemia (blood clots) most often (Source: G Perceau).
 |
| Source: https://www.hindawi.com/journals/crin/2019/1630613/ |
 |
| Source: https://www.hindawi.com/journals/crin/2019/1630613/ |
My first initial "signs" of Calciphylaxis. These images are of my buttocks. It felt like small rocks (what I later learned where calcifications) under my skin. It was painful to the touch. (March 2018)
Bruising and spreading and the beginning stages of necrosis. (April 2018)
Scabbing & hardening of the ulcers. May 2018
Wound Vac. May 2018
Trauma to my heel during my stay in the burn unit caused the Calciphylaxis to spread to my heel. Making it impossible to walk. June 2018
Debriding and Skin Graft Surgeries - I went through 11+ surgeries. 2018



Skin graft healing in burn unit. 2018
Why did I get Calciphylaxis?
The cause of Calciphylaxis remains obscure. Most cases occur in the setting of chronic renal failure (99% of patients get this from dialysis), abnormal calcium-phosphate homeostasis, and hyperparathyroidism (Source: MedScape).
Recent studies have revealed that most people with the condition have abnormalities in blood-clotting factors. These abnormalities can lead to small blood clots forming more often than they normally would. People with Calciphylaxis have an imbalance in the metabolism of calcium. This causes calcium to be deposited in the smallest parts of the arteries (arterioles), which eventually leads to the formation of blood clots in the arterioles. Blood clots can cause fat tissues and skin to be deprived of oxygen and nourishment (Source: Mayo Clinic).
Patients at an increased risk appear to be those who are obese and those who have been exposed to immunosuppressive agents.
Calciphylaxis occurs more frequently in areas where body fat is most abundant, such as the thighs, the buttocks, and the lower part of the abdomen.
(Source: MedScape)
Risk Factors:
Calciphylaxis most commonly affects people who have end-stage kidney failure.
Possible risk factors include:
- Obesity
- Diabetes
- Abnormalities in blood-clotting factors
- Long-term dialysis and sometimes kidney transplantation
- An imbalance of calcium, phosphorus and aluminum in the body
- Some medications, such as warfarin (Coumadin, Jantoven), calcium-binding agents or corticosteroids
- An overproduction of parathyroid hormone (PTH), which regulates the level of calcium and phosphorus in the body — a condition known as hyperparathyroidism
- Uremia, a toxic condition in which substances normally eliminated in the urine — such as calcium and phosphorus — build up in the body
How is it diagnosed?
Skin biopsy. Blood tests. Imaging studies.
To diagnose Calciphylaxis, your doctor may remove a small tissue sample from an area of affected skin for analysis (deep wedge skin biopsy). Multiple biopsies may be necessary, with a risk of propagating Calciphylaxis (Source: DermNet NZ).
Blood samples measure a variety of substances in your blood — calcium, phosphorus, parathyroid hormone, abnormalities in blood-clotting factors, aluminum, urea nitrogen, creatinine and albumin, among others — to help your doctor assess your kidney and liver function. X-rays may show branch-like calcium deposits in the blood vessels (vascular calcifications) that are common in Calciphylaxis and in other advanced kidney diseases. (Source: Mayo Clinic)
How is it treated?
Dialysis. Medications. Surgery. Intensive Wound Treatment. Pain Management.
A medication called sodium thiosulfate (STS) can decrease calcium buildup in the arterioles. It's given intravenously three times a week, usually during dialysis. This takes 3-6 months to see if it does anything. Your doctor may also recommend a medication called Cinacalcet (Sensipar), which can help control parathyroid hormone (PTH), if it applies to you.
Your doctor will evaluate your current medications and eliminate potential triggers for Calciphylaxis, such as warfarin, corticosteroids or iron, and may modify the amount (dose) of your calcium or vitamin D supplements.
If an overactive parathyroid gland (hyperparathyroidism) contributes to abnormal calcium metabolism by producing too much PTH, surgery to remove all or part of the parathyroid glands may be recommended.
Emphasize compliance with the dialysis prescription. Education regarding dietary restrictions and the need for phosphate binders (Source: MedScape).
Complications:
These include:
- Severe pain
- Large, deep, non-healing ulcers (chronic & extensive)
- Blood infections
- Secondary infection with sepsis
- Death, usually due to infection and multi-organ failure
Typically, the outlook for people with Calciphylaxis isn't hopeful. Early detection and treatment is very important in helping to prevent serious infections (Source: Mayo Clinic).
How to prepare for your appointments: (taken from Mayo Clinic website)
When you make the appointment, ask if there's anything you need to do in advance, such as fasting before having a specific test. It's also a good idea to bring a family member or friend with you because it can be difficult to remember all of the information from your appointment.
It's also helpful to make a list of:
- Your symptoms, including any that seem unrelated to the reason for your appointment
- Key personal information, including major stresses, recent life changes and family medical history
- All medications, vitamins or other supplements you take, including the doses
- Questions to ask your doctor
For Calciphylaxis, some basic questions to ask your doctor include:
- What's likely causing my symptoms?
- Are there other possible causes for my symptoms?
- What tests do I need?
- Is my condition likely temporary or long lasting?
- What treatment do you recommend?
- I have other health conditions. How can I best manage these conditions together?
- Are there any dietary restrictions I need to follow?
- What's my prognosis?
- Are there brochures or other printed material I can have? What websites do you recommend?
- What to expect from your doctor
Your doctor is likely to ask you several questions, such as:
- When did your symptoms begin?
- Have your symptoms been continuous or do they come and go?
- How severe are your symptoms?
- Does anything seem to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
To get the best results and answers to your questions, you must advocate for yourself. If you can't advocate for yourself, bring someone who will/can. Always remember, medical professionals are simply doing their jobs...their jobs that you (in essence) have hired them to do. They work FOR YOU - to make YOU better. It is okay to tell medical professionals 'no' if you feel like the suggested methods/treatments/medicine is not for you. The best thing you can do is equip yourself with as much knowledge as possible to better articulate your needs.
Once the actual disease is treated, then what?
Once Calciphylaxis is treated, under control, and no longer spreading, your main focus will be skin & wound care and pain management.
Wound Care:
Meticulous wound management is essential to prevent infection and speed healing. The deep ulcers are necrotic and are stubborn to heal, so patience and consistency is key. (I'm still healing 2+ years later.)
- Surgically remove or debride the necrotic tissue (particularly if moist) – sometimes this means a limb must be amputated.
- Keep wounds clean.
- Systemic antibiotics are indicated if clinically infected.
Wounds have a weird odor?
Certain dressings like hydrocolloids tend to produce a characteristic odor as a result of the chemical reaction that takes place between the dressing and wound exudate. While not directly harmful to the patient, wound odor is often indicative of bioburden or other barriers to wound healing. Certain bacteria that colonize wounds and release compounds can also cause odor. (Source: Wound Source)
Though there is no universally recognized scale for measuring wound odor, the following can be used to qualitatively assess wound odor for documentation purposes:
- Very strong: Odor is evident on entering the room (6–10 feet or 2–3 meters from the patient) with the dressing intact.
- Strong: Odor is evident on entering the room (6–10 feet or 2–3 meters from the patient) with the dressing removed.
- Moderate: Odor is evident at close proximity to the patient when the dressing is intact.
- Slight: Odor is evident at close proximity to the patient when the dressing is removed.
- No odor: No odor is evident, even at the patient’s bedside with the dressing removed.
(Source: Haughton and Young (1995) - Wound Source)
Personal recommendations for wound care:

Hydrocolloid Dressings
Petroleum Gauze
Dakin's solution (used to prevent and treat skin and tissue infections that could result from cuts, scrapes and pressure sores)
Microcyn® (a safe hypochlorous acid based antimicrobial treatment for the cleansing, irrigation and moistening of wounds)
Curel Itch Defense Shower Body Wash
Shea Moisture In-Shower Body Conditioner
Povidone Iodine Prep Solution
Silvasorb Gel
Silver Sulfadiazine Cream
Silicone Cream
Z-Guard Paste
INZO Skin Protectant Cream
Calmoseptine Ointment
Hydrogel
Gentamicin Sulfate Ointment
Mupirocin Antibiotic Ointment
Aquaphorn Healing Ointment
Weleda Skin Food
Comfortable clothing (I live in pajamas and sweats)
Plush blankets (I have become incredibly sensitive to textures against my skin. I prefer anything soft/fuzzy/silky to the touch.)
Pain Management:
(Source: BC Renal Agency)
Can this be prevented?
There is no known way how to prevent Calciphylaxis. However, patients with chronic renal failure, on dialysis, or with hyperparathyroidism tend to be more susceptible to developing Calciphylaxis. These signs are some identifiable causes of Calciphylaxis in some patients.
Testimonials of loved ones and survivors of Calciphylaxis (from online support group):
 "My mom's doctor first time around diagnosed it properly. Second time around they said gangrene. I kept begging for STS (sodium thiosulfate) but nope the surgeon was convinced it was gangrene. She passed away 7 weeks ago but lived 2 years after the first go round with proper treatment.”
"My mom's doctor first time around diagnosed it properly. Second time around they said gangrene. I kept begging for STS (sodium thiosulfate) but nope the surgeon was convinced it was gangrene. She passed away 7 weeks ago but lived 2 years after the first go round with proper treatment.”"They said it would take three to six months to see if it (STS) helps. I am so scared. I couldn't bear losing my sister.”
"It's possible to beat it if you have the right professionals and they listen. Fight like hell. I did the first time. This time with COVID-19 it added a layer because I couldn't be as present (for my loved one). Don't let it stop you. Fight and fight more."
"Many general doctors will not know about this disease...it is so uncommon and generally hits people who have kidney dialysis. My sister has it...I told my general doc about it and she ha[d] to look it up as well--and she is a great doctor."
 "One year ago today, my wife passed from this horrible disease...worst week of my life because I knew the battle was lost but couldn't bring myself to tell my kids until 3 days before she passed.... I remember her begging the doctor for just a little more time and it brought him to tears...the last week the bruises would pop up, break open and become hard scabs within a hour...she begged me not to watch but I couldn't stop...I climbed in bed with her on the last day and told her we will be fine."
"One year ago today, my wife passed from this horrible disease...worst week of my life because I knew the battle was lost but couldn't bring myself to tell my kids until 3 days before she passed.... I remember her begging the doctor for just a little more time and it brought him to tears...the last week the bruises would pop up, break open and become hard scabs within a hour...she begged me not to watch but I couldn't stop...I climbed in bed with her on the last day and told her we will be fine.""They told me she was going to make it until the day before she died. She developed a problem with her liver and died the next morning. It was the most terrible thing to watch. This is a barbaric disease. I’m so sorry for anyone who developed it. I feel it had something to do with her taking Warsfin."
Recommended hospitals that have experience with Calciphylaxis & Kidney Disease:
UCSF Medical Center
Santa Clara Valley Medical Center
Boston Medical Center
Massachusetts General Hospital
Mayo Clinic
Cleveland Clinic
Lehigh Valley Health Network
University of Missouri Health Care - Columbia
Stanford Medicine (Stanford University)
Good Samaritan Hospital
Penn Medicine (University of Pennsylvania Hospital)
Einstein Health
UHealth (University of Miami Health System)
Michigan Medicine (University of Michigan Health)
Sources:
- Personal Experience
- Actual Real Life Testimonials from Caregivers and Survivors from Online Support Group
- http://www.bcrenalagency.ca/resource-gallery/Documents/BCPRAEOLChampionTrainingPainAssessmentManagmentHan.pdf
- https://www.mayoclinic.org/diseases-conditions/calciphylaxis/symptoms-causes/syc-20370559
- https://emedicine.medscape.com/article/1095481-overview
- https://dermnetnz.org/topics/calciphylaxis/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4696752/
- https://www.hindawi.com/journals/crin/2019/1630613/
- https://www.ncbi.nlm.nih.gov/pubmed/8304650
- https://stanfordmedicine25.stanford.edu/blog/archive/2016/can-you-diagnose-this-rare-skin-condition.html
- https://www.ajkd.org/article/S0272-6386(04)00420-2/pdf
- https://www.woundsource.com/patientcondition/wound-odor
- https://www.sciencedirect.com/science/article/pii/S0151963815004536?via%3Dihub
If you have any questions, concerns, or comments feel free to leave them below in the comments section. Please note: I am not a medical professional and information found on this page is not to substitute being seen by a medical professional. This page is to serve as an informational guide and resource.


























I wish we had all this information under one umbrella when going through the journey. Thank you for taking the time to share your journey and for sharing the extensive research you have collected.
ReplyDeleteThank you
ReplyDeleteThis comment has been removed by a blog administrator.
ReplyDeleteMy friend is located in the Houston area with terrible calciphylaxis sores all over his lower back region. He is 47 and strong, although recently on dialysis and has diabetes. I do not feel like the hospital is pushing hard enough - they've basically told him there is nothing more to do but wait to die. I've looked online for Houston based specialists and have emailed those in Boston but with no luck. Any leads on someone in Houston that is well versed in this disease and its treatment?
ReplyDelete